
Copyright © 2024. All rights reserved. | sitemap


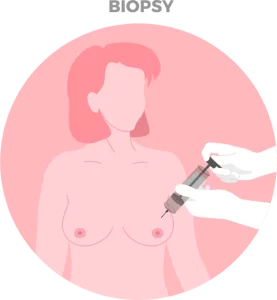 Most masses seen on mammograms are benign (not cancerous). When a cancer is suspected, a needle biopsy of the breast mass is required to obtain tissue for microscopic analysis. Additional biopsy and placement of small marking clips inside the breast tissue (to locate the area of concern) may be required to confirm if enlarged/suspicious lymph nodes under the arm have been affected by the cancer.
Upon confirmation of the breast cancer diagnosis, additional testing will be performed to understand the subtype, tumour grading, expression of hormone receptors (estrogen and progesterone) and HER2 protein. These factors will aid the breast cancer specialist in creating a management plan for the patient.
Except for very small breast cancers, patients should undergo additional staging scans to determine the extent (or spread) of the cancer. Imaging that may be used include CT (computed tomography), bone scan, PET or MRI.
Most masses seen on mammograms are benign (not cancerous). When a cancer is suspected, a needle biopsy of the breast mass is required to obtain tissue for microscopic analysis. Additional biopsy and placement of small marking clips inside the breast tissue (to locate the area of concern) may be required to confirm if enlarged/suspicious lymph nodes under the arm have been affected by the cancer.
Upon confirmation of the breast cancer diagnosis, additional testing will be performed to understand the subtype, tumour grading, expression of hormone receptors (estrogen and progesterone) and HER2 protein. These factors will aid the breast cancer specialist in creating a management plan for the patient.
Except for very small breast cancers, patients should undergo additional staging scans to determine the extent (or spread) of the cancer. Imaging that may be used include CT (computed tomography), bone scan, PET or MRI.
 b). Hormonal Therapy
b). Hormonal Therapy
The Cancer Centre @ Paragon
290 Orchard Road #17-05/06
Paragon Medical (Lobby F)
Singapore 238859
The Cancer Centre @ Mount Elizabeth Orchard
3 Mount Elizabeth #12-11
Mount Elizabeth Medical Centre
Singapore 228510
(by appointment only)
The Cancer Centre @ Mount Elizabeth Novena
38 Irrawaddy Road #07-41
Mount Elizabeth Novena Specialist Centre
Singapore 329563

BOOK AN APPOINTMENT
Incorporated in 2005, Singapore Medical Group (SMG) is a healthcare organisation with a network of private specialist providers across four established pillars - Aesthetics, Diagnostic Imaging & Screening, Oncology and Women's and Children's Health. Within Singapore, SMG has more than 40 clinics strategically located in central Singapore and heartland estates. Beyond Singapore, SMG also has an established presence in Indonesia, Vietnam and Australia. Learn about our privacy policy here.
