Share This:

Ms JK, a Chinese woman in her 40s was overwhelmed by conflicting emotions.
First to hit home was the shock of her diagnosis of breast cancer.
Then followed the relief from knowing that the diagnosis was made at an early stage and that surgery with conservation of her breast was a possibility.
Finally, came the fear and confusion caused by well-meaning friends and relatives who counselled her to undergo a total removal of her breast instead as it was “safer”.
As you can imagine, this was an emotional roller-coaster for Ms JK.
When in shock after the diagnosis of breast cancer, most patients think, almost intuitively, that removing the whole diseased breast would be better than removing just the cancerous lump.
Surgery for total removal, called mastectomy, would be safer and carry a lower risk of a relapse than that for partial removal, called lumpectomy, they think.
As the Chinese saying goes: When cutting grass, remove the roots or it will grow again.
Makes sense, right? Wrong.
I explained to Ms JK: “You can have your cake and eat it too. There is no conflict between conserving the breast and avoiding a relapse.”
Seeing that she was not quite convinced, I figured that changing her mind about something that is counter-intuitive would take a great deal of explanation.
Broadly speaking, we can look upon treatment of breast cancer in its early stages as a two-pronged strategy.
The first prong involves treating the affected breast and its immediate surroundings.
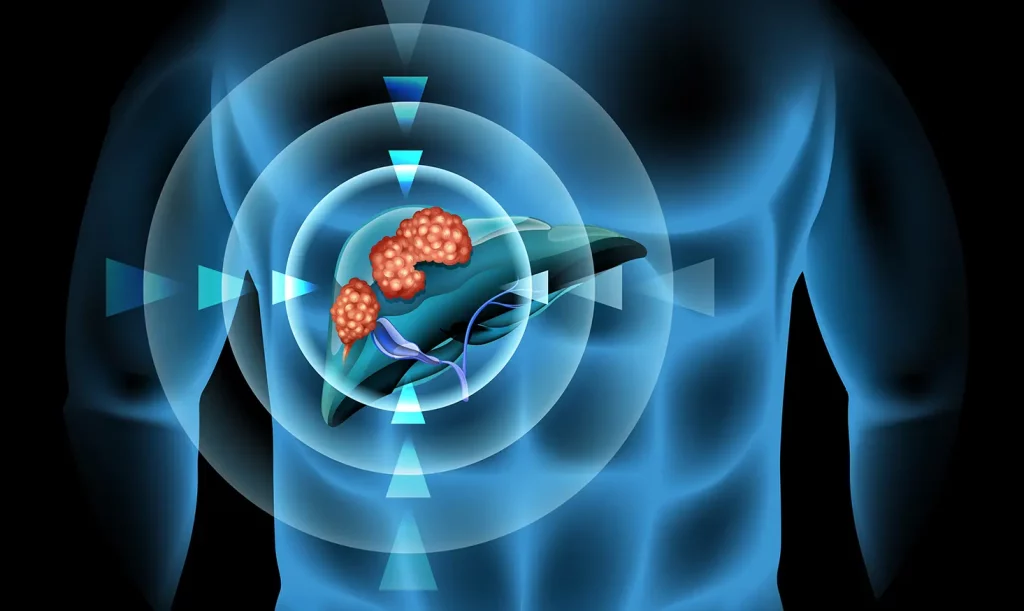
This is done usually through surgery to remove the cancer, aided by radiation [high- energy X-ray beams], to destroy cancer cells is the immediate surroundings that the naked eye cannot see.
The other prong is treatment of the whole body – through chemotherapy and hormonal therapy – to purge any breast cancer cells that may have spread to other parts such as the lungs or liver, but are too few to be detected even with the best form of medical imaging available today.
This small number of surviving cancer cells may trigger a relapse in the months and years that follow.
Chemotherapy is the use of drugs that are capable of killing cancer cells.
They are administered into the body by direct infusion into the blood or orally. They circulate through the bloodstream and reach all parts of the body, thereby fulfilling their role of destroying cancer cells that have spread from the breast and lodged elsewhere.
Hormonal therapy is based on treatment that deprives breast cancer of the stimulatory effects of female hormones in the body that frequently drive its growth.
If a patient initially diagnosed with early-stage breast cancer were to, unfortunately, have a relapse, more often than not, the failure is in the treatment of the whole body that rather than that of the breast and its immediate surroundings.
That is the reason at the point of relapse, most women have an advanced form of the cancer that has spread to many parts of the body.
Put simply, when breast cancer does come back, it does not come back in the breast.
For this reason, the modern approach to treatment of potentially curable breast cancer leans towards a more conservative approach to surgery and a more aggressive approach to chemotherapy. It focuses on improving “whole body control”, where, one might argue, the battle is won or lost.
Hence, the trend is to remove just the cancerous lump in the breast, followed by radiation, rather than to remove the whole breast. There is a similar trend towards removing only the lymph node most likely to be affected by the cancer, rather than all the lymph nodes in the armpit adjacent to the affected breast.
We have understood that more mutilating surgery does not necessarily lead to a better chance of a cure. On the other hand, chemotherapy given before or after surgery is stave off the return of the cancer is becoming more intense. After I explained this to Ms JK, I could tell from her changing expression that she was beginning to use the light.
To make the surgery easier to perform and to get better cosmetic results, I started her on chemotherapy first to shrink the breast cancer to a small size and mop up any cancer cells hiding in other parts of the body.
This was followed by surgery, which removed the cancerous lump successfully and also conserved her breast.
Ms JK was very grateful that she got the information which helped her make the right choice for herself.
Thinking conservation is the way to go. Doctors, too, should go “green”.

At The Cancer Centre (TCC), Dr Wong Seng Weng and his medical oncology team are focusing their expertise on implementing preventive measures, actively conducting screening and providing innovative, targeted treatments for adult cancers, as well as using proven technologies to ensure optimal patient safety and comfort.
Dr Wong, a visiting consultant medical oncologist at Mount Elizabeth Hospital (Novena) and Mount Elizabeth Hospital (Orchard), holds the appointment of Adjunct Clinician Scientist at the Institute of Bioengineering and Nanotechnology in the Agency of Science, Technology and Research (A*STAR). He is also an active member of the American Society of Clinical Oncology, European Society of Medical Oncology and Singapore Society of Oncology.
Share This:



















The Cancer Centre @ Paragon
290 Orchard Road #17-05/06
Paragon Medical (Lobby F)
Singapore 238859
The Cancer Centre @ Mount Elizabeth Orchard
3 Mount Elizabeth #03-04
Mount Elizabeth Medical Centre
Singapore 228510

BOOK AN APPOINTMENT
Incorporated in 2005, Singapore Medical Group (SMG) is a healthcare organisation with a network of private specialist providers across four established pillars - Aesthetics, Diagnostic Imaging & Screening, Oncology and Women's & Children's Health. Within Singapore, SMG has more than 40 clinics strategically located in central Singapore and heartland estates. Beyond Singapore, SMG also has an established presence in Indonesia, Vietnam and Australia. Learn about our privacy policy here.
