
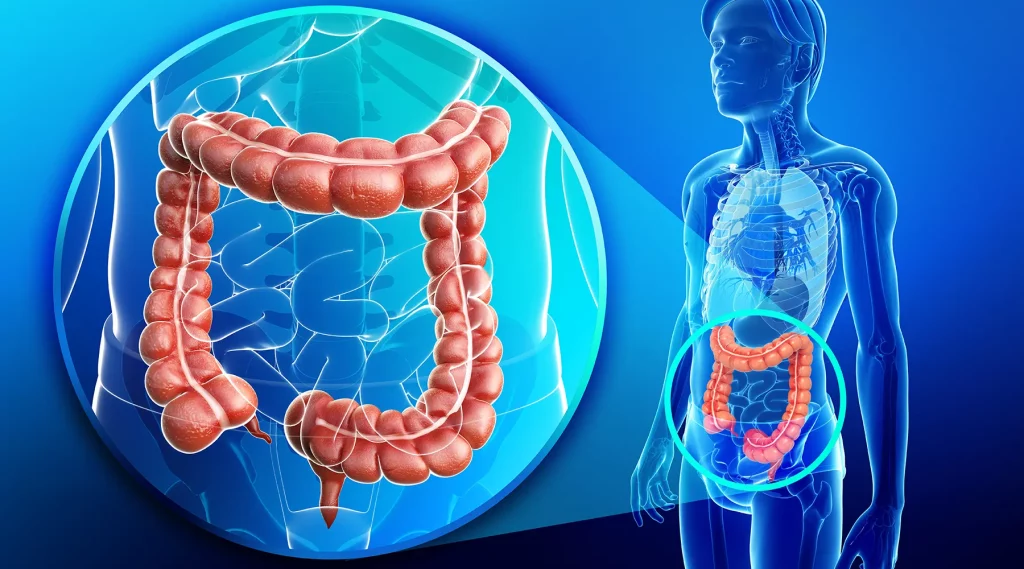
Colorectal cancer refers to cancer that starts in the colon or rectum. Cancer occurs when there is an uncontrolled growth of cells. Typically, colorectal cancers begin from benign growths (polyps) on the inner lining of colon or rectum. Not all polyps will turn into cancer, but adenomatous (cancers that begin in cells that produce mucus and other fluids) polyps may have the potential to grow into colorectal cancer after many years.
More than 95% of colorectal cancers are adenocarcinomas. Very rarely, cancers of colon and rectum are due to carcinoid tumours, gastrointestinal stromal tumours (GIST), lymphomas or sarcomas. This writeup refers to colorectal adenocarcinomas.
Colorectal cancer is very prevalent in Singaporeans. In fact, it is the most common cancer in Singaporean men and the 2nd most common cancer in Singaporean women1. Furthemore, Singaporean men have the highest incidence of colorectal cancers within Southeast Asia, with incidence rates as high as western countries2.
Every day, 3 Singaporean men and 2 Singaporean women are diagnosed with colorectal cancers1. Of great concern is the increase in the global incidence trend of colorectal cancers in adults younger than 50 years old. The National Cancer Institute’s SEER Registry (USA) showed the incidence of colorectal cancer is increasing at 2% per year3. More than two-thirds of colorectal cancers in younger adults are not associated with a family history of colorectal cancers and tend to be diagnosed at later stages while requiring a more aggressive clinical course.
In general, colorectal cancers begin when healthy cells in the colon develop changes (mutations) in their DNA. Usually, many changes in DNA over time are required to cause cells to grow out of control.
Most of these DNA changes are sporadic and poorly understood. Certain modifiable risk factors increase the chance of acquiring these DNA changes. They include:
There are risk factors that cannot be controlled including:
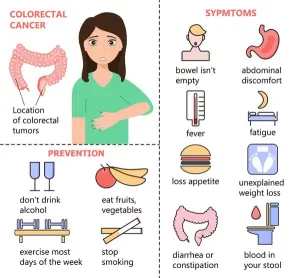
Colorectal cancers may present with:
However, most early-stage colorectal cancers generally have little to no symptoms when the growth is small. Hence, screening for polyps and cancers remains the single most effective strategy in decreasing the mortality from colorectal cancers.
Screening for colorectal cancer means testing healthy, at-risk people, who have no symptoms. The idea is to identify polyps and cancer at the early stage so that intervention bears the highest chance of cure. Unfortunately, in Singapore, only about 2 in 5 individuals who are 50 to 69 years of age go for colorectal cancer screening at the recommended frequency.
There are various screening methods developed for colorectal cancer, with each test having its own pros and cons.
The Singapore Cancer Society has rolled out annual complimentary Faecal Immunochemical Test (FIT) kits to all Singaporeans and permanent residents aged above 50.5 FIT is cheap, simple, non-invasive and can be self-administered at home without needing any dietary modification. However, it needs to be done annually and any abnormal results will need to be followed up with colonoscopy to exclude polyps or cancers.
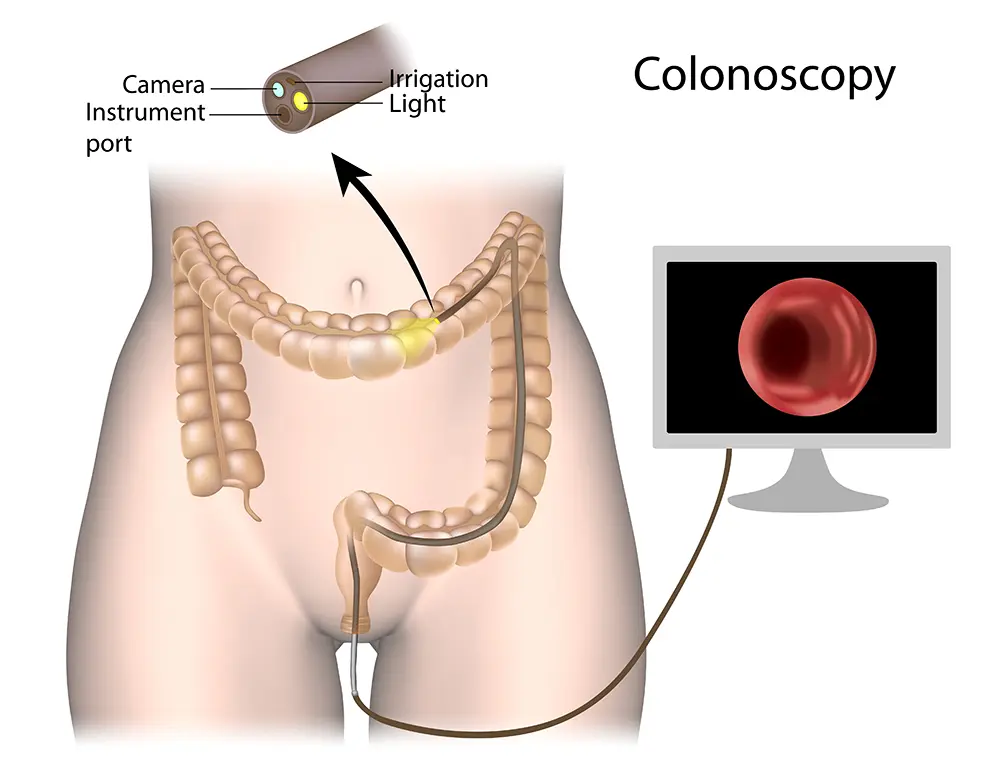
A proper visual inspection of the colon will require prior bowel emptying using laxatives to clean the colon.
A colonoscope (flexible tube with light source at the tip) is inserted by a doctor through the anus along the whole length of the colon to look for polyps or cancers. Any abnormal spot can be sampled using a small instrument passed through the colonoscope. Light sedation is usually administered prior to the procedure to keep you comfortable.
A sigmoidoscope is used to examine the rectum and sigmoid colon and allows sampling of any suspicious lesion. Only the last 60cm of the rectum/colon is visualised.
A CT machine rotates around the body and takes many images of the abdomen. Special computer software then recreates 3-dimensional images of the inside of the colon and rectum, which allows the doctor to look for polyps and cancer. However, any suspicious lesions cannot be sampled and patients with abnormal results will need to undergo a formal colonoscopy.
For average-risk individuals, most guidelines recommend colorectal cancer screening to start from 50 years onwards. In 2018, the American Cancer Society lowered the age to start colorectal screening to 45 years old. For individuals at higher risk of colorectal cancer due to personal or family history of polyps / colorectal cancer or underlying genetic syndromes, screening and preventive measures need to be personalised and start a lot earlier.
Colorectal cancers are diagnosed formally by colonoscopy and biopsy of any suspicious mass seen. Occasionally, patients present with stage 4 disease and have other accessible sites that are amenable to biopsy under radiological guidance without needing to undergo bowel preparation.
Once the diagnosis of colorectal cancer is confirmed, staging tests will need to be done to determine the stage of cancer and an appropriate treatment plan. Commonly, patients will be asked to undergo some basic blood tests and additional scans.
For rectal cancer, MRI rectum will be helpful to determine the extent of local structures / lymph nodes involvement. CT scan or PET scan will be helpful to exclude distant spread of the cancer.
 Appropriate treatment of colorectal cancer depends on:
Appropriate treatment of colorectal cancer depends on:
Stage 1 colorectal cancers are generally treated with surgery alone. Some stage 2 colon cancer with adverse features on surgical specimens may require chemotherapy after surgery (adjuvant chemotherapy) to reduce the risk of relapse. Patients with stage 3 colon cancers are generally advised to undergo adjuvant chemotherapy after surgery. Stage 4 colon cancers are generally treated with chemotherapy, targeted therapies or immunotherapy. Select patients with stage 4 colon cancer who have limited spread, especially in the liver or lungs, may be suitable for curative intent surgery /local ablation plus chemotherapy. Radiotherapy has a well-defined role prior to surgery in locally advanced rectal cancer, to improve local control and reduce local recurrence. It can also be used to ablate limited sites of metastatic disease.
Surgery is the main treatment for early stage colorectal cancer. It is also used in metastatic settings if there is bowel obstruction or major bleeding. It involves the removal of the tumour and nearby lymph nodes. Hemicolectomy (removal of part of the large intestines that contain the tumour together with a small segment of normal intestines) is the usual procedure. The remaining healthy colon is usually joined up during the same surgery. Keyhole surgery is becoming the standard for suitable patients as the recovery time is much shorter without compromising on cancer outcome.
A colostomy is where the colon is brought up to an opening in the abdominal skin. It may be required in cases of bowel obstruction that is not amenable to stenting or rectal cancer surgery to allow better healing of the reattached colon downstream. A minority of patients with underlying genetic conditions or severe inflammatory bowel disease may require total colectomy where the whole length of the colon is removed.
Radiation therapy is the use of high energy rays to destroy cancer cells. Radiotherapy may be used in the following circumstances:
Locally advanced rectal cancer that is being considered for surgery may benefit from upfront radiotherapy (usually in combination with chemotherapy) prior to surgery to reduce local recurrence rate. Delivery of radiotherapy treatment prior to surgery is better tolerated than radiotherapy after surgery and associated with no increase in surgical complications.
For select patients with small lesions in suitable locations, local ablation of the lesion using stereotactic body radiation therapy (SBRT) may allow good cancer control in a non-invasive method. This is achieved by delivering a very intense and precise dose of radiotherapy while minimising damage to normal surrounding tissues.
May help to improve symptoms such as pain / bleeding from bulky cancer pressing on vital structures.
Chemotherapy is the use of anti-cancer drugs that works in various ways to induce cancer cells death. There are many chemotherapy drugs that are effective for colorectal cancer in both oral and intravenous preparation. Chemotherapy is given in varying cycles (schedules), typically over every 2-3 weeks. Adjuvant chemotherapy given after surgery is typically given for up to 6 months. In a metastatic setting, chemotherapy is typically combined with targeted therapy. Side effects of chemotherapy vary and most drugs in colorectal cancer do not lead to major hair loss, severe vomiting or major impairment in the immune system. Your doctor will be able to manage and guide you through the chemotherapy side effects with supportive medications.
Immunotherapy involves the administration of intravenous antibodies to boost immune recognition and killing of cancer cells. Approximately 3-5% of patients with inoperable stage 4 colon cancer have a deficiency in DNA mismatch repair (dMMR). Based on recent data from Keynote-177 trial, single agent Pembrolizumab is superior to first line chemotherapy with fewer side effects and much more durable response8. Immunotherapy may also be beneficial in patients with high tumour mutation burden (TMB) as defined by next-generation sequencing of tumour tissues.
Colorectal cancer is a common cancer in Singaporean men and women. There is also a rising trend for a younger age of onset. Appropriate screening tests aim to identify precancerous polyps and early stage colorectal cancers, with the goal of increasing the chances of long-term cure. There have been major advancements in the treatment of colorectal cancer with better treatment selection tools, better chemotherapy and targeted therapy, more modern surgical and radiotherapy techniques and better supportive care. Consult our oncologists for colorectal cancer treatment in Singapore.
The Cancer Centre @ Paragon
290 Orchard Road #17-05/06
Paragon Medical (Lobby F)
Singapore 238859
The Cancer Centre @ Mount Elizabeth Orchard
3 Mount Elizabeth #03-04
Mount Elizabeth Medical Centre
Singapore 228510

BOOK AN APPOINTMENT
Incorporated in 2005, Singapore Medical Group (SMG) is a healthcare organisation with a network of private specialist providers across four established pillars - Aesthetics, Diagnostic Imaging & Screening, Oncology and Women's & Children's Health. Within Singapore, SMG has more than 40 clinics strategically located in central Singapore and heartland estates. Beyond Singapore, SMG also has an established presence in Indonesia, Vietnam and Australia. Learn about our privacy policy here.
