A small proportion of prostate cancers are due to genetic predisposition. Patients who carry germline mutations in their DNA-repair genes are more likely to develop prostate cancer, regardless of whether they have a family history of prostate cancer. These mutations are built into the genes, and hence can be passed down to children.
4.6% of patients with localised prostate cancer have these genetic mutations, while 11.8% of patients with metastatic prostate cancer have the mutations.2 Localised prostate cancer means the cancer is confined to the prostate gland, whilst metastatic cancer means that the cancer has spread beyond the prostate gland.
Those with a positive family history for prostate cancer are at higher chance of contracting cancer. Having a first-degree relative (such as a father or brother) with prostate cancer increases a man’s risk of having prostate cancer in the future.

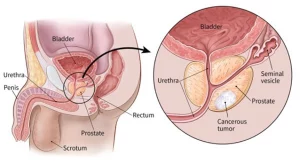
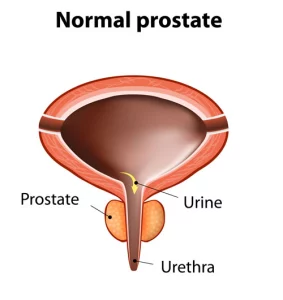

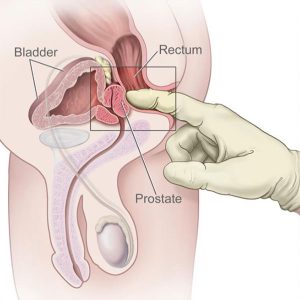
 Image from Cancer Research UK
Image from Cancer Research UK Image from Prostate Cancer Foundation of Australia
Image from Prostate Cancer Foundation of Australia
